Analytical X-Ray Safety Manual
Contents
- Regulatory Chain for Radiation-Producing Equipment
- Machine Use Authorizations (MUA)
- Units of Radiation Measurement
- Radiation Protection Standards
- Table 1 - Fatalities from Accidents in Different Occupations
- Biological Effects of Ionizing Radiation
- Radiation Exposure Limits and Comparisons
- Dosimetry
- Fundamental Health Physics Principles
- Radiation Monitoring
- Machine Inspection Parameters
- Cabinet General Safety Protocol
- Diffraction/Fluorescence General Safety Protocol
- Electron Microscope General Safety Protocol
- References
Regulatory Chain for Radiation-Producting Machines
Nuclear Regulatory Commission (NRC)
Code of Federal Regulations, Title 10
State of California, Department of Health Services, Radiologic Health Branch
California Code of Regulations, Title 17
University of California, Davis
Radiation Safety Program
Office of Environmental Health and Safety
Health Physics Section
UC Davis Radiation Safety Manual
Machine Use Authorization (MUA)
Authorized Machine Use Personnel
All Authorized Machine Use Personnel Must:
- Post areas where radiation-producing machines are used and stored. Rooms housing x-ray equipment must have warning signs on entrances specifically for x-ray.
- Maintain security/control of ionizing radiation-producing equipment. Equipment itself or rooms housing x-ray equipment must be locked when not in use.
- Keep a log of dates, use parameters, and users' names, as well as any performance checks done on equipment. The Office of Environmental Health and Safety will also monitor work areas where x-ray machines are used to detect leakage or scatter radiation.
- If you modify, transfer, dispose of, or purchase x-ray equipment, the California Department of Public Health must be advised by the Office of Environmental Health and Safety of these facts. Notify Environmental Health and Safety (530-752-1493) of these changes.
- Wear dosimetry (film badges and/or finger rings) to document radiation exposures while working with x-ray equipment.
Machine Use Authorizations (MUA)
Requests to use radiation-producing equipment are separated into the following categories:
-
Analytical Use
-
Diagnostic Human and Non-Human Use
Separate machine use applications are required for each machine, see Section IX (Forms) of the Radiation Safety Manual for a sample application of Form 30. The Principal Investigator must consult with the campus or medical center Radiation Safety Officer prior to completing any application for the use of a radiation-producing machine. There may be requirements for additional shielding or state certification
Units of Radiation Measurement
Activity (Unit: Curie)
Since the discovery by William Roentgen in 1895 that energetic electrons impinging on a target of high atomic number produce rays that easily penetrate matter and can expose photographic film (X rays), the scientific community has adopted special units to describe the amount and nature of ionizing radiation.
The International Commission on Radiological Units (ICRU) was formed to develop a system of units and nomenclature specific to the needs of physicians and other persons working with not only X rays, but other types of radiation found in nature or produced by man. The units that have been developed were named after pioneers in the field (Roentgen, Curie) or began as descriptive terms that turned into acronyms, then into units (rem-"roentgen equivalent man"). The ICRU designated units on the basis of observed quantities. Thus the special unit of activity, the curie, was equal to the number of disintegrations taking place per unit time from 1 gram of radium. The curie (Ci) was later redefined as the activity of that quantity of radioactive material in which the number of disintegrations per second is 3.7E10 (a number nearly the same as the number of disintegrations per second from 1 gram of radium).
We have since learned that a Curie of any radioisotope is a very appreciable amount, too great for most laboratory applications, so we commonly find activity expressed as millicurie (mCi, 1E-3 Curie) or microcurie (µCi, 1E-6 Curie). It is essential that one not confuse the symbol for micro with that for milli. The 1,000-fold error that results may mean the difference between an almost inconsequential radiation problem and a major radiation hazard. A useful number to remember is 2.22E6 disintegrations per minute per microcurie. Most tracer applications require microcurie quantities, although it is not unusual to find millicurie quantities of 3H, 32P, and 125I in many laboratories.
Exposure ( Unit: Roentgen)
The ICRU defined the special unit of exposure in air to be the Roentgen (symbolized by R). R = 2.58E-4 coulomb kg air This unit is special in that it is defined only for X or gamma radiation in air. Thus, the Roentgen is not applicable to alphas, betas, or neutrons. Many survey instruments provide output data in terms of mR/hr (mR, 1E-3R). The Roentgen is not always useful for making accurate evaluations of energy absorbed due to radiation impinging on material. It is the absorbed energy that is a true index of biological damage. If one knows how well a certain material can absorb radiation as compared with air, the energy absorbed by that material when exposed to 1 R can be calculated. It is very easy to measure ionization in air with inexpensive equipment, so that the Roentgen can be measured directly. It is not so easy to measure the energy absorbed in material directly.
Absorbed Dose (Unit: rad)
The rad is the special unit of absorbed energy. It is defined as that amount of ionizing radiation that deposits 100 ergs/gram of material. The rad is applicable to all types of ionizing radiation, yet it is difficult to measure directly. Normally ionization in air or another gas is measured and the absorbed dose in a particular material calculated. One Roentgen results in 87.7 ergs being absorbed in 1 gram of air; if muscle tissue is placed in the same radiation beam, 1 R in air corresponds to about 95 ergs/gram. For most applications of x rays and gamma rays, it is reasonable to assume that 1 R = 1 rad. One Roentgen is a large exposure, therefore, we more often see the term millirad (mrad, 1E-3 rad).
Dose Equivalent (Unit: rem)
The rem is the unit of dose equivalent. The dose equivalent accounts for the difference in biological effectiveness of different types of radiation. It is the product of the absorbed dose (rad) times the quality factor (QF) of the radiation. The quality factor for x, gamma, and beta radiation is 1, therefore for these radiations 1 rad = 1 rem. The quality factor for alpha radiation is 20 and the quality factor for neutron radiation varies with energy from 2-11.
Radiation Protection Standards
Introduction
Radiation protection standards apply to radiation workers or the general population. Standards for the general population are of importance since they serve as a basis for many of the considerations applicable to the siting of nuclear facilities and the design and implementation of environmental surveillance programs. Included in this section are a brief history of the development of radiation protection standards, a review of the goals and objectives sought, and a description of the approach being used to base such standards on the associated risk.
History of the Basis for Dose Limits
Shortly after the discovery of x-rays of 1895 and of naturally occurring radioactive materials in 1896, reports of radiation injuries began to appear in the published literature (i). Recognizing the need for protection, dose limits were informally recommended with the primary initial concern being to avoid direct physical symptoms. As early as1902, however, it was suggested that radiation exposures might result in delayed effects, such as the development of cancer. This was subsequently confirmed for external sources and, between 1925 and 1930, it became apparent for internally deposited radionuclides when bone cancers were reported among radium dial painters (1).
With the publication by H.J. Muller in 1955 (ii) of the results of his experiments with Drosophila, concern began to be expressed regarding the possibility of genetic effects of radiation exposures in humans. This concern grew and dominated the basis for radiation protection from the end of World War II until about 1960, and led to the first consideration of recommendations for dose limits to the public. With the observances of excess leukemia among the survivors of World War II atomic bombings in Japan, and the failure to observe the previously anticipated genetic effects, however, the radiation protection community gradually shifted to a position in which somatic effects, primarily leukemia, were judged to be the critical (or governing) effects of radiation exposures. This belief continued until about 1970 when it was concluded that, although somatic effects were the dominating effects, the most important such effects were solid tumors (such as cancer of the lung, breast, bone, and thyroid) rather than leukemia (iii). Finally, in 1977 the International Commission on Radiological Protection (ICRP) initiated action to base radiation protection standards on an acceptable level of the associated risk (iv). This effort was provided additional support by the National Council on Radiation Protection and Measurements (NCRP) with the issuance of their updated "Recommendations on Limits for Exposure to Ionizing Radiation" in 1987 (v).
Basic Standards - Philosophy and Objectives
The primary source of recommendations for radiation protection standards within the United States is the National Council on Radiation Protection and Measurements (NCRP). Recommendations of this group are in general agreement and many of them have been given legislative authority through publication of the Code of Federal Regulationsvi by the U.S. Nuclear Regulatory Commission.
- Basic Philosophy-As a general approach, the main purposes in the control of radiation exposures are to ensure that no exposure is unjustified in relation to its benefits or those of any available alternative; that any necessary exposures are kept as low as is reasonably achievable (ALARA); that the doses received do not exceed certain specified limits; and that allowance is made for future developments.
- Objectives of the Guides-In general, the objective or goal of radiation protection (and associated standards) is to limit the probability of radiation-induced diseases in exposed persons (somatic effects) and in their progeny (genetic effects) to a degree that is reasonable and acceptable in relation to the benefits of the activities that involve such exposures.
Radiation-induced diseases of concern in radiation protection are classified into two general categories: stochastic effects and non-stochastic effects.
-
A stochastic effect is defined as one in which the probability of occurrence increases with increasing absorbed dose, but the severity in the affected individuals does not depend on the magnitude of the absorbed dose. A stochastic effect is an all-or-none response as far as individuals are concerned. Cancers (solid malignant tumors and leukemia) and genetic effects are examples of stochastic effects.
-
A non-stochastic effect is defined as a somatic effect which increases in severity with increasing absorbed dose in the affected individuals, owing to damage to increasing numbers of cells and tissues. Examples of non-stochastic effects attributable to radiation exposure are lens opacification, blood changes, and decreases in sperm production in the male. Since there is a threshold dose for the production of non-stochastic effects, limits can be set so that these effects can be avoided.
Radiation Protection Standards:
- Occupational Dose Limits
Standards provide for an upper boundary effective dose equivalent limit of 50 mSv/year (5 rem/year). On a cumulative basis, however, the newest NCRP recommendations have proposed that the average cumulative effective occupational dose equivalent not exceed 10 mSv (1 rem) times the age of the worker. UC Davis guidelines limit exposure to roughly one-half the state and federal limits. Two key changes or factors to be noted relative to these recommendations are:
- The dose limit applies to the sum of the doses received from both external and internal exposures.
- The standards are expressed in terms of the effective dose equivalent, an approach which permits, on a mathematical basis, the summation of partial and whole body exposures.
Dose Limits for the General Population
For a variety of reasons, dose limits for the general population are set lower than those for radiation workers. Justifications for this approach include the following:
- The population includes children who might represent a group of increased risk and who may be exposed for their whole lifetime.
- It was not the decision or choice of the public that they be exposed.
- The population is exposed for their entire lifetime; workers are exposed only during their working lifetime and presumably only while on the job.
- The population in question may receive no direct benefit from the exposure.
- The population is already being exposed to risks in their own occupations; radiation workers are already being exposed to radiation in their jobs.
- The population is not subject to the selection, supervision, and monitoring afforded radiation workers.
- Even when individual exposures are sufficiently low so that the risk to the individual is acceptably small, the sum of these risks (as represented by the total burden arising from somatic and genetic doses) in any population under consideration may justify the effort required to achieve further limitations on exposures.
Concept of Effective Dose Equivalent (4,5)
A. Basic Objectives:
The objective in developing the concept of the effective dose equivalent was to obtain a system that would provide a unit for radiation protection standards that could be used to express, on an equal risk basis, both whole body and partial body exposures. In developing this approach, the ICRP sought to:
- Base the limits on the total risk to all tissues as well as the hereditary detriment in the immediate offspring (first two generations);
- Consider, in the case of internally deposited radionuclides, not only the dose occurring during the year of exposure, but also the committed dose for future years.
Having stated this objective, the next goal of the ICRP was to set the R occupational dose limits at such a level that the risks to the average worker incurred as a result of his/her radiation exposure would not exceed the risk of accidental death to an average worker in a "safe" non-nuclear industry.
Based on a review of data on a world-wide basis (see Table I), the ICRP concluded that, on the average, within a "safe" industry about 100 workers or less would be killed accidentally each year for one million workers employed. Thus, the associated risk of accidental death to the average worker in a "safe" industry would be about: 100/year/1,000,000 = 1E-4/year.
B. Risks of Death from Radiation Exposures:
Based on epidemiological studies with human populations and biological studies in animals, estimates can be made of the risk of a fatality from cancer or a genetic death for given levels of dose equivalent to various body organs. Some examples are given below to illustrate the thinking that goes into formulation of risk factors:
- Studies of the survivors of the atomic bombings in Japan at the close of World War II indicate that for a collective dose of 10,000 person-Sv (1,000,000 person-rem) to the bone marrow, there will be, after latency period, an average of one excess case of leukemia occurring in the population each year. Assuming that each such case ultimately results in a death, and that the excess continues for a period of 20 years, there will be a total of 20 excess cases of leukemia and, therefore, 20 excess deaths due to this exposure. Thus, the risk of death due to leukemia resulting from exposure of the bone marrow can be estimated to be: 20 excess person deaths/10,000 person-Sv = 2E-3/Sv
- Similar studies among uranium miners have shown that there will be approximately 20 excess cases of lung cancer (and consequently 20 excess deaths, assuming all cases of lung cancer are fatal) for each 10,000 person-Sv (1,000,000 person-rem) to the lungs. Thus the risk of death from lung cancer can be estimated to be: 20 excess deaths/10,000 lung-Sv = 2E-3/Sv
- For breast cancer, epidemiological data have shown that there is an excess of about 100 breast cancers per 10,000 person-Sv (1,000,000 person-rem) to the female breasts. Assuming that breast cancer is fatal 50% of the time; and assuming that the population being exposed consists of 50% men and 50% women, then the risk of excess deaths due to exposure to the female breasts can be estimated to be: 100 excess cancers/10,000 breast-Sv x (0.5 fatality rate) x (0.5 of population being female)= 2.5E-3 / Sv
- For thyroid cancer, epidemiological data have shown that there is an excess of about 100 thyroid cancers per 10,000 Sv (1,000,000 rem) to the thyroids in humans. However, the fatality rate for thyroid cancer is only about 5%, so the risk of death due to cancer of the thyroid resulting from exposure to ionizing radiation is: 100 excess cancers/10,000 thyroid-Sv x (0.05 fatality rate)=5E-4/Sv
Similar calculations can be made to estimate the excess deaths due to exposures of other body organs, as well as genetic deaths due to exposure of the reproductive organs.
Table 1 - Fatalities from Accidents in Different Occupations
Fatalities From Accidents in Different Occupations (x 10,000 Per Year)
| Category | Occupation | Fatalities per Year |
|---|---|---|
| Safe | Trade | 0.5 |
| Safe | Manufacturing | 0.6 |
| Less Safe | Service | 0.7 |
| Less Safe | Government | 0.9 |
| Less Safe | Transportation & Utilities | 2.7 |
| Less Safe | Construction | 3.9 |
| Less Safe | Agriculture | 4.6 |
| Less Safe | Mining & Quarrying | 6.0 |
| Less Safe | Sport | 15 |
| Less Safe | Deep Sea Fishing | 30 |
| Less Safe | High-Rise Steelworkers | 50 |
| Less Safe | Farm Machinery Workers | 80 |
Biological Effects of Ionizing Radiation
Physical and Chemical Effects of Ionizing Radiation
- Ionizing radiation is so named because its initial interaction with matter is the ejection of an orbital electron from an atom, forming a pair of ions with opposite charges. Radiation passing through living cells will ionize or excite atoms and molecules in the cell structure. This produces ions and radicals within the cell (mostly from water molecules). When these radicals and ions interact with other cell materials, damage can result. Certain levels of cellular damage can be repaired by the cell. Further levels can result in cell death.
- May directly involve and damage biologically important molecules in the cell - Direct Effects. Damage to the DNA molecule or a chemical change in other cellular material are the primary results. Damage to the DNA molecule can result in somatic mutations that may show up years after the exposure or genetic mutations that require several life spans to appear.
- May initiate a chain of chemical reactions, mediated through cellular water, leading to ultimate biologic damage - Indirect Effects. An hydroxyl poisoning effect on the cell membrane results in a change in its permeability. Inactivation and release of enzymes is the primary result.
- The unit of radiation dose is the rad which equals 100 ergs of energy absorbed per gram of tissue.
- Biological effects of all types of ionizing radiations are similar. Some radiations are more efficient than others, however, and produce more biological damage per rad dose.
- The rem is the unit of biological dose called the units of Dose equivalence) which takes into consideration the differing efficiencies of the different radiations.
- The Dose Equivalence in rems is obtained by multiplying the dose in rads by the Quality Factor (QF) of the particular radiation. The QF is related to its ionization density.
1 for most gamma and x-rays, beta particles
2 - 11 for neutrons
20 for alpha particles
Cellular Effects of Ionizing Radiation
- Cell killing is responsible for acute somatic effects of radiation. It occurs by two mechanisms:
- Inhibition of mitosis which results from moderate doses and leads to delayed cell death.
- Immediate cellular death which results from very high doses.
- Alteration of cellular genetic material consistent with continued cell proliferation: Usually manifests no visible change in cellular appearance but a point (recessive) mutation is formed, which may or may not be passed to future generations.
Systemic Biological Effects of Ionizing Radiation
- Somatic effects:
Abnormality may become manifest only after many generations of cell replication: proposed mechanism for long-term somatic effects of radiation - carcinogenesis, nonspecific life shortening. (These are non-stochastic effects.)
- Genetic effects:
If involves gonadal cells, mutations are passed on to offspring. Increase in number of "recessive" mutations in population pool leads to increased probability of abnormalities in offspring due to chance mating of individuals carrying same mutation. (These are stochastic effects.)
Acute Somatic Effects of Radiation Exposure in Humans
- Related to killing of cells, generally in tissues where cells are rapidly proliferating. Observed effects usually occur 1-3 weeks after radiation exposure.
- Systems of primary involvement:
- Hematopoietic system - (fever, infections, hemorrhages)
Chief organ: bone marrow
Symptom latency: days to weeks
Death threshold: less than 500 rem
Characteristic symptoms: Malaise, fever, fatigue, infection, hemorrhage, and anemia. Low counts of platelets, lymphocytes and erythrocytes result in low resistance to infection and a decreased clotting ability.
- Gastrointestinal system - (abdominal pain, vomiting, severe diarrhea, fluid and electrolyte imbalance)
Chief organ: small intestine
Symptom latency: hours to days
Death threshold: 500-2000 rem
Characteristic symptoms: Malaise, nausea, vomiting, diarrhea, fever, dehydration, G.I. malfunction, and electrolyte loss. The intestinal epithelium is destroyed.
- General systemic effects "radiation sickness" - (central nervous system syndromes.
Chief organ: brain
Symptom latency: minutes to hours
Death threshold: 2000-5000 rem
Characteristic symptoms: lethargy, tremors convulsions, encephalitis, meningitis, and edema. Acute inflammation and vascular damage results in neuronal functional impairment.
- Hematopoietic system - (fever, infections, hemorrhages)
Dose relationships
- 0-150 rem - none to minimal symptoms. Perhaps long-term effects many years later.
- 150-400 rem - moderate to severe illness due to hematopoietic derangement.
- 400-800 rem - severe illness. LD50 in man probably about 500 rem. GI damage at higher doses.
- Above 800 rem - 100% fatal, even with best available treatment.
Partial body exposure
Effects depend on particular tissue or organ exposed, but significant acute changes are usually seen only after a fairly high radiation dose (>1000 rem).
Long-Term Effects of Exposure to Ionizing Radiation
- General characteristics: Usually occur many years after acute or chronic radiation exposure.
- Biologic Effects of Ionizing Radiation:
- Occur with much lower dosesand dose-rates: insufficient to cause acute somatic effects.
- Probably related to irreparable damage to genetic material in cells which are capable of continued cell division.
Radiation Carcinogenesis in Humans
Genetic and proliferative alterations of cells require years to many lifetimes to develop.
- Tumor development: Ionizing radiation in large amounts is an effective carcinogenic agent.
- Sterility: Temporary sterility can be induced at exposure levels of approximately 150 rem. Females are more often permanently affected than males.
- Cataracts: Due to the high sensitivity of the lens of the eye, opaque areas of the lens develop after exposure of 200-600 rem.
- Life-shortening: The aging process is increased. Nutrition to the cell appears to be impaired. The total cell number is decreased and there is a modification of the composition of cellular material.
- Fetal damage: The fetus is highly radiosensitive due to the rapid division of cells. No measurable fetal damage has been seen at exposures less than one rem.
- Chromosomal damage: Detection of chromosomal damage requires many generations. An Oak Ridge study suggests that low intensity (1-10 rem/day) continuous exposure has only 1/4 - 1/10 the mutagenic efficiency of acute exposures.
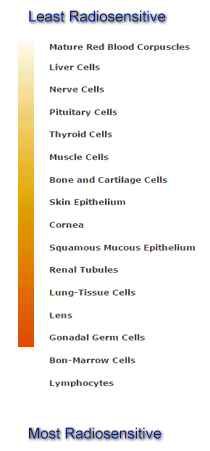
Law of Bergonie and Tribondeau
Radiation sensitivity of cells generally varies directly with the rate of proliferation and the number of future divisions, and inversely with the degree of morphological and functional differentiation.
The following is listed from least to most radiosensitive:
Factors that Influence the Severity of Absorbed Dose
- Internal Radiation
- Amount of Radioactivity
- Radioisotope
- Nature or type of the emission
- Critical Organ
- Physical half-life
- Biological half-life
- Age, weight, sex
- External Radiation
- Amount of Radioactivity
- Nature or type of the emission
- Radiation Energy
- Time
- Distance
- Shielding
- Age, weight, sex
- Area of the Body Exposed
Radiation Exposure Limits and Comparisons
Dose Equivalent Limits (Monitored Radiation Workers)
| Target Tissue | Regulatory Limit | UC Davis Guideline |
|---|---|---|
| Whole Body | 5,000 mrem/year | 2,500 mrem/year |
| Extremities | 50,000 mrem/year | 25,000 mrem/year |
| Skin of the Whole Body | 50,000 mrem/year | 25,000 mrem/year |
| Fetus | 500 mrem/gestational period | 50 mrem/month |
Common Radiation Exposures
(Natural Sources and Human Made)
| One Coast to Coast Flight | 3 mrem |
| Natural Background Radiation in the U.S. | 150 - 300 mrem/year |
| Chest Radiograph, A/P View | 2 mrem/view |
| Chest Radiograph, Lateral View | 10 mrem/view |
| Screening Mammography (film/screen combination) | 40 mrem/view |
| Computerized Tomography of Body | 1,000 mrem |
Biologically Significant Radiation Exposures
(Absorbed/Acute Exposure)
| Risk of Contracting Cancer Increased 0.05% | 1,000 mrem |
| Temporary Blood Count Change | 50,000 mrem |
| Permanent Sterilization in Men | 350,000 mrem |
| Permanent Sterilization in Women | 250,000 mrem |
| Skin Erythema | 200,000 mrem |
| Cataract Formation | 50,000 mrem |
Dosimetry
Dosimeters are devices that quantitate the amount of radiation to which a person has been exposed.
Types of Dosimetry Used on Campus
-
Film Dosimeters
The dosimeter used most often on campus is the film badge, comprised of one of two small x-ray films enclosed within a light-tight envelope and plastic holder. The badge is worn from one to four weeks on the trunk of the body, usually at waist level or on the collar. Photographic film in the form of thin, even layers of emulsion is spread on a thick paper support base. The emulsion consists of small silver halide crystals embedded in a gelatin matrix. When the badge is exposed to radiation, energy is transferred to the emulsion causing silver ions to cluster together. These silver clumps are called latent image centers. This film detects x and gamma rays, beta particles greater than 1 MeV, and neutron radiation, except fast neutrons. Fast neutrons require a separate type of film. the amount of exposure is related to the length of the track that is left on the film. The accuracy of film badges is plus or minus 10 mrem.
There are two types of film badges. One badge monitors x, gamma and beta radiation. The other contains an additional film which is sensitive to neutrons. Each holder has filters on the from and back sides containing an open window, then plastic aluminum, cadmium, and lead filters. The type of radiation (i.e., x, gamma, beta, or neutron) can be determined by observing the relative darkening of the film behind each filter.
-
Thermoluminescent Dosimeters (Whole Body Exposure Monitors)
In some situations, thermoluminescent dosimeters containing lithium fluoride or calcium fluoride chip and powder cartridges are used in place of x-ray film as a personnel monitor. Exposure of these materials to ionizing radiation results in the trapping of electrons in energy levels above those occupied normally. When the dosimeter is heated, these electrons are liberated from the traps. As the electrons return to their normal levels, visible light is released. The amount of light released is measured and is proportional to the exposure of the dosimeter to radiation. These materials are x, beta, and gamma sensitive and exposure is reported as being either deep and/or shallow energy penetration.
-
Finger Ring Dosimeters
To monitor hand exposure to radioactive materials thermoluminescent dosimeters in the form of finger rings are worn on the dominant hand with the TLD chip facing the source of radiation. The TLD process is described above. It is important to assure chip placement in the dosimeter prior to each use.
The dosimetry reporting company, an independent contractor, will report exposures per individual for the finger ring and deep and/or shallow energy penetration for the whole body.
Precautions on Use of Dosimetry
When not in use, store your dosimetry in an area free of ionizing radiation. If you lose, contaminate, get your badge or rings wet or leave them in the sun for an extended period of time, please notify the campus Office of Environmental Health and Safety, Health Physics or the UCDMC Health Physics Office. While wearing a lead apron, place your badge outside the apron.
-
Film badges
Fading of the latent image centers is produced with time, high humidity, and high temperature.
-
TLD
The lithium fluoride chips and powder are highly sensitive to heat and moisture.
Distribution and Use of Film Badges
-
Dosimetry is issued by the campus Office of Environmental Health and Safety, Health Physics (530-752-1493) or the UCDMC Health Physics Office (916-734-3355) based on procedures used and the type of equipment used.
-
Badges may be exchanged weekly, monthly, or quarterly, depending upon the type of equipment or type and amount of materials used and experimental design.
-
Both the campus and UCDMC Health Physics sections document the dosimetry readings for you and the California Department of Public Health, Radiologic Health Branch.
Dosimetry Records
All dosimetry records are on file with the Office of Environmental Health and Safety, Health Physics. Upon your request, EH&S will supply you with your dosimetry history. If at any time your exposure exceeds the campus guidelines or is unusually high, a health physics staff member will notify you of the incident.
Fundamental Health Physics Principles
Factors in Maintaining ALARA
The ALARA concept in radiation protection is to keep your radiation exposure as low as reasonably achievable. You can limit your exposure to radiation by using the three methods of (1) time, (2) distance, and (3) shielding.
Time
Reducing the time of exposure is a very practical method of radiation protection. The longer the time exposed to a radiation field, the greater the total exposure. The standards for permissible levels of radiation in unrestricted areas and how time influences them is outlined below 1.
A. Radiation levels which, if an individual were continuously present in the area, could result in a dose in excess of two millrems in any one hour; or
B. When an exposure rate exceeds 2 millirem per hour, calculations must be made to determine how long an individual can remain in the area.
Distance
Distance is a very effective shielding measure and often the least expensive means of radiation protection. As one moves away from the source of radiation the amount of radiation at a given distance from the source is inversely proportional to the square of the distance (inverse square law).
|
ID2 = id2I = intensity at a distance (D) from a point source i = intensity as a different distance (d) from the same point source |
Shielding
Shielding is also a practical means of radiation protection. For alpha and beta radiation, very little shielding is required to absorb the emissions completely.
-
alpha stopped by paper
In general, as the density and/or thickness of a shielding material increases, the absorption of radiation emissions by the material also increases. Usually, the higher the atomic number of the shielding material, the higher its density.
Radiation Shielding
Half value layer - the thickness of a material that decreases the x-ray beam intensity by one-half.
| Energy (keV) | Air (cm) | Water (cm) | Al (cm) | Lead (cm) |
| 10 | 115 | 0.1 | 0.01 | 5E-04 |
| 20 | 765 | 0.9 | 0.07 | 7E-04 |
| 30 | 1648 | 1.9 | 0.22 | 2E-03 |
| 40 | 2319 | 2.6 | 0.43 | 4E-03 |
| 50 | 2766 | 3.1 | 0.67 | 8E-03 |
Radiation Monitoring
Personnel Monitoring
-
Whole Body Badge (Film or TLD)
-
Measures radiation dose equivalent to individual
-
IS NOT a protective device.
-
-
Finger Ring (TLD)
-
Measures radiation dose equivalent to hand.
-
IS NOT a protective device
-
Radiation Level Surveys
-
Thin Window GM Survey Meter
-
Detection of leakage radiation.
-
Positive indication of the production of x-rays.
-
Useful in monitoring routine operations.
-
ALWAYS USE THIN WINDOW for low energy x-rays.
-
-
Annual Environmental Health and Safety Radiation Protection Survey
-
Check for leakage radiation
-
Check for compliance with campus and State regulations.
-
Check personnel lists.
-
Machine Inspection Parameters
University of California, Davis
Office of Environmental Health and Safety
ANALYTICAL X-RAY SYSTEM AUDITS
| MUA #:______Principal Investigator:_____________Department:_________________
Analytical Machine Type:____________ Location:_____________UC Davis Inventory #:_____ Control Manufacturer:___________ Control Model:__________Control Serial #:____________ Tube Manufacturer:____________Tube Model:____________ Tube Serial #:_______________ (X) : Non-Compliance or Check mark to the right of column = Satisfactory [na - not applicable] |
POSTING
| ( ) (500) Notice to Employees (rev. 10/94) | ( ) (501) Area posted |
| ( ) (502) Control warning label | ( ) (503) EH&S Safety Protocol (rev. 10/96) |
Comments:____________________________________________________________
PERSONNEL
| ( ) (504) MUA personnel list accurate | ( ) (505) Dosimetry worn |
| ( ) (506) Whole body badge issued | ( ) (507) Finger ring issued |
Comments:______________________________________________________________
TRAINING
| ( ) (522) PI training provided | ( ) (523) PI training outline adequate |
| ( ) (524) Survey meter training provided | ( ) (525) Users attended EH&S training |
Comments:_______________________________________________________________
MACHINE INFORMATION
| ( ) (508) Warning lights operable | ( ) (509) Warning lights adequate |
| ( ) (510) Interlock operable | ( ) (511) Interlock adequate |
| ( ) (512) kVp meter operable | ( ) (513) mA meter operable |
| ( ) (514) Timer indicator operative | ( ) (515) Breaker box adequate |
Comments:________________________________________________________________
CONTROLS
| ( ) (516) Room security adequate | ( ) (517) Machine security adequate |
| ( ) (518) Machine location satisfactory | ( ) (519) Operational survey instrument |
| ( ) (520) Usage log contents | ( ) (521) Usage documented |
Comments:________________________________________________________________
X-RAY SURVEY
| ( ) (527) Reading within unrestricted limits | |
| Type of target: | Meter used: |
| Meter calibration date: | Background reading: |
| kVp setting: | mA setting: |
Sketch the X-ray system on the back side and record survey results.
DIFFRACTION OR FLUORESCENCE X-RAY MACHINE
| ( ) (528) Shutter warning signal/light | ( ) (529) Shutters operative (without signal?) |
| ( ) (530) Unused ports mechanically secure | ( ) (531) Bypass key protocol followed |
Comments:_________________________________________________________________
MISCELLANEOUS
| ( ) (532) Safety protocol or owner's manual exists | ( ) (533) Violation of EH&S safety protocol |
| ( ) (534) Radiation incident | ( ) (535) Other (i.e., Violation of UCD Policy) |
Comments:_________________________________________________________________
Audit Performed By:__________________________________ Date:__________________
ADDITIONAL AUDIT ISSUES FOR DIFFRACTION OR FLUORESCENCE X-RAY UNITS
-
Principal Investigator (PI) Training of Authorized Users
-
Inspect the PI's training program (outline/content)
-
When and how is the power supply turned off?
-
-
Dosimetry
-
What is the MUA policy for wearing dosimetry?
-
-
Safety Interlocks
-
What is the MUA policy for entering the interlocked area?
-
When the interlock circuit integrity is broken, does the power supply turned off?
-
List all the warning indicators and their purpose.
-
-
Operating/Emergency Procedures
-
Summarize the MUA operating procedure.
-
Summarize the MUA emergency procedure. (Is it the EH&S Safety Protocol?)
-
-
Sample Changing Procedures
-
Describe the authorization's procedure for changing samples.
-
Is it a written procedure?
-
Is a sample change recorded in the usage log?
-
When and how is the power supply turned off?
-
-
Maintenance, Modification and Disassembly
-
Describe the MUA procedure for any maintenance, modification or disassembly.
-
Who is authorized to modify the machine?
-
How often is the camera realigned?
-
How often is the X-ray beam realigned?
-
Describe the procedure for a realignment.
-
-
Survey Meter
-
When is the survey meter used?
-
-
Security
-
How is the machine secured from unauthorized use?
-
Who controls the security key to the room/machine?
-
What is the procedure for obtaining and/or using the security key?
-
Who has access to the room/machine?
-
Safety Interlock Override Key Control
-
Is the machine provided with a safety interlock override key?
-
What is the procedure for obtaining and/or using the key?
-
Who has access to the key?
-
Does the principal investigator oversee the key?
If not, who is the key custodian and what qualifies them as custodian?
-
How is security of the key maintained?
-
Appropriate radiation safety officer signature approving key custodian. ______________
-
- Comments___________________________________________________________________
- MUA:____________
- Auditor:__________________________________________
- Date:________________________
Cabinet General Safety Protocol
UNIVERSITY OF CALIFORNIA, DAVIS
OFFICE OF ENVIRONMENTAL HEALTH AND SAFETY, HEALTH PHYSICS
X-ray Cabinet General Safety Protocol
Machine Identification:
Manufacturer:______________________________________________ Model:_________________
Principal Investigator:________________________________________ Phone:________________
General Safety Regulations:
-
Cabinet units may only be operated by personnel on the Machine Use Authorization. All authorized personnel must receive instruction in and demostrate an understanding of the operation of the machine before starting unsupervised work.
-
Whole body and finger ring dosimetry is required for all personnel working with cabinet units.
-
DO NOT use the safety interlock to turn the machine off; use the main switch.
-
DO NOT override the safety interlock unless there is an approved written procedure.
-
Make sure the machine is OFF before changing samples; always check the current and voltage meters and/or use a survey meter to detect x-rays.
-
Do not modify the built-in shielding. If modifications must be made, contact the Office of Environmental Health and Safety in order for a unit and operation safety survey.
-
Cabinet units must be secured against unauthorized use. This can be accomplished through key control of the unit or the room
-
An operating log must be maintained that includes the following information for each use of the unit:
-
Date
-
Operator
-
Beam voltage and current
-
Time on and off (or total exposure time)
-
-
Notify the Office of Environmental Health and Safety immediately in the event of any abnormal personnel radiation exposure.
-
Changes in the location or disposition of diffraction/fluorescence units must have the approval of the Office of Environmental Health and Safety. Notify EHS prior to the acquisition, disposal, or transfer of any diffraction/fluorescence unit.
-
Contact EHS for information regarding radiation safety or radiation survey instrumentation. A copy of the California Radiation Control Regulations is available at EHS.
Diffraction/Flourescence General Safety Protocol
UNIVERSITY OF CALIFORNIA, DAVIS
OFFICE OF ENVIRONMENTAL HEALTH AND SAFETY, HEALTH PHYSICS
X-ray Diffraction/Fluorescence General Safety Protocol
Machine Identification:
Manufacturer:______________________________________________ Model:_________________
Principal Investigator:________________________________________ Phone:_________________
General Safety Regulations:
-
Diffraction/fluorescence units may only be operated by personnel on the Machine Use Authorization. All authorized personnel must receive instruction in and demostrate an understanding of the operation of the machine before starting unsupervised work.
-
Whole body and finger ring dosimetry is required for all personnel working with diffraction/fluorescence units.
-
DO NOT use the safety interlock to turn the machine off; use the main switch.
-
DO NOT override the safety interlock unless there is an approved written procedure.
-
Make sure the machine is OFF before changing samples; always check the current and voltage meters and/or use a survey meter to detect x-rays.
-
No operation involving removal of covers, shielding materials, or tube housings; or modifications to shutters, collimators or beam stops must be performed without ascertaining that the tube is off and will remain off until safe conditions have been restored. Use the main switch; do not rely on the safety interlock.
-
Check radiation scatter with a survey meter after each realignment. Notify the Office of Environmental Health and Safety immediately in case of unusually high readings. Call the Office of Environmental Health and Safety for a radiation protection survey after any machine modification that may change the radiation output or shielding effectiveness.
-
Diffraction/fluorescence units must be secured against unauthorized use. This can be accomplished through key control of the unit or the room
-
An operating log must be maintained that includes the following information for each use of the unit:
-
Date
-
Operator
-
Beam voltage and current
-
Time on and off (or total exposure time)
-
-
Notify the Office of Environmental Health and Safety immediately in the event of any abnormal personnel radiation exposure.
-
Changes in the location or disposition of diffraction/fluorescence units must have the approval of the Office of Environmental Health and Safety. Notify EHS prior to the acquisition, disposal, or transfer of any diffraction/fluorescence unit.
-
Contact EHS for information regarding radiation safety or radiation survey instrumentation. A copy of the California Radiation Control Regulations is available at EHS.
Electron Microscope General Safety Protocol
UNIVERSITY OF CALIFORNIA, DAVIS
OFFICE OF ENVIRONMENTAL HEALTH AND SAFETY, HEALTH PHYSICS
Electron Microscope General Safety Protocol
Machine Identification:
Manufacturer:______________________________________________ Model:_________________
Principal Investigator:________________________________________ Phone:_________________
General Safety Regulations:
-
Electron microscopes may only be operated by personnel trained and approved by the Principal Investigator responsible for the unit
-
Electron microscopes must be secured against unauthorized use. This can be accomplished through key control of the unit or the room
-
An operating log must be maintained that includes the following information for each use of the unit:
-
Date
-
Operator
-
Beam voltage and current
-
Time on and off (or total exposure time)
-
-
Do not modify the built-in shielding and viewing ports. If modifications must be made, contact the Office of Environmental Health and Safety for a safety survey of the unit.
-
Notify the Office of Environmental Health and Safety immediately in the event of any abnormal personnel radiation exposure.
-
Changes in the location or disposition of electron microscopes must have the approval of the Office of Environmental Health and Safety. Notify EHS prior to the acquisition, disposal, or transfer of any electron microscope.
-
Contact EHS for information regarding radiation safety or radiation survey instrumentation. A copy of the California Radiation Control Regulations is available at EHS.
References
-
Slobodien, M. "Radiation Hazards in the Laboratory," in Laboratory Safety: Theory and Practice, Fuscaldo, A.A., Erlick, B.J. and B., eds., Academic Press, New York, 1980.
-
Moeller, Dade W., "Occupational and Environmental Radiation Protection," Harvard School of Public Health, (August 1987).
-
Bushong, Stewart C.: Radiologic Science for Technologies, Ed. 3, St. Louis, 1984, The C.V. Mosby Co.
-
Bushong, Stewart C.: Radiologic Science for Technologies, Ed. 3, St. Louis, 1984, The C.V. Mosby Co.
-
Eisenbud, M., Environment, Techology, and Health; Human Ecology in Historical Perspective, New York University Press, New York, NY (1978).
-
Muller, H.J., "Radiation and Human Mutation, " Scientific American, Vol. 193, No. 5 (1955).
-
"The Effects on Populations of Exposure to Low Levels of Ionizing Radiation, " Advisory Committee on the Biological Effects of Ionizing Radiation, Report No. 3, National Academy Press, Washington, D.C., (1980).
-
"Recommendations of the International Commission on Radiological Protection, " Publication 26, International Commission on Radiological Protection, Annals of the ICRP, Vol. 1, No. 3 (1977).
-
"Recommendations on Limits for Exposure to Ionizing Radiation, " National Council on Radiation Protection and Measurements, Bethesda, MD (1987).
-
"Standards for Protection Against Radiation," Title 10, Part 20, Code of Federal Regulations (1993).
General References
-
National Academy of Sciences/National Research Council, "The Effects on Populations of Exposure to Low Levels of Ionizing Radiation," Report of the Advisory Committee on the Biological Effects of Ionizing Radiation, U.S. Government Printing Office, Washington, D.C. (1980).
-
"Federal Research on the Biological and Health Effects of Ionizing Radiation," National Academy Press, 2101 Constitution Avenue, N.W., Washington D.C., 20418 (1982).
-
National Council on Radiation Protection and Measurements, "Influence of Dose and Its Distribution in Time on Dose-Response Relationships for Low-LET Radiations, NCRP Report No. 64, 1790 Woodmont Avenue, Bethesday MD 20814 (1980).
-
National Council on Radiation Protection and Measeurements, "Review of NCRP Radiation Dose Limit for Embryo and Fetus in Occupationally Exposed Women," NCRP Report No. 53, 1790 Woodmont Avenue, Bethesda MD 20814 (1977).
-
Brill, A.B. (Editor), Low-Level Radiation Effects: A Fact Book, The Society of Nuclear Medicine, 475 Park Avenue South, New York, NY (1985).